HISTORY OF PRESENTING ILLNESS:
- A 67 year old female patient came to the OPD with C/O shortness of breath (SOB) since 1/2 hour.
- She had H/O heartburn like episodes since a year. They were relived without use of any medication.
- She has H/O TB diagnosed 7 months ago for which she completed the course of medication a month ago.
- Patient was apparently asymptomatic till 9pm on that day (27/4/21). She apparently ate dinner and slept. When she woke up at night for washroom she developed sweating on exertion and shortness of breath even at rest.
- No H/O chest pain, palpitations, giddiness, nausea, vomiting, LOC, pedal oedema, decrease in urine output,PND.
- No H/O fever, cough, cold, sore throat.
PAST HISTORY:
- K/C/O of DM2 since 12 years and is on Rx GLIMI M2 PO/BD
- K/C/O of hypertension since 6 months and is on Rx TELMA 20 mg PO/OD
- H/O pulmonary TB 7 months ago when she had cough, chest pain. Completed the course for TB a month ago. Currently negative for TB.
FAMILY HISTORY:
- No significant family history
PERSONAL HISTORY:
- She had mixed diet with normal appetite,
- Adequate sleep,
- Regular bowel and bladder movements
- And no addictions.
EXAMINATION:
- On examination, the patient was conscious, co-operative, coherent.
- Patient was oriented to time, place and person.
- VITALS: ( Upon admission)
- BP- 130/80 mm Hg
- PR- 126 BPM
- Afebrile
- CVS- S1, S2 +, no murmurs
- Respiration- B/L, Inspiratory crepts +, dyspnoec
- Sp O2- 96%
- GRBS- 256 Mg/dl
- P/A- Soft, Bowel sounds +
- CNS- NAD
INVESTIGATIONS-
1) An ECG was done upon admission. The ECG shows NSTEMI ( acute coronary syndrome)
An ECG will show the following characteristics for an NSTEMI:
- depressed ST wave or T-wave inversion
- no progression to Q wave
- partial blockage of the coronary artery
2) A chest X-Ray was taken in another hospital on the next day.
3) A chest CT scan was taken in another hospital the following day.
PROVISIONAL DIAGNOSIS- Acute coronary syndrome (NSTEMI)
Treatment at hospital-
- Upon seeing the ECG, the patient was given TAB MET XL 25 MG/STAT.
- The patient was then advised to shift to a HC for PCI upon explaining to the patient’s attender about the patient’s condition.
- The patient was then taken to another hospital, for further treatment but PCI was not done as there were no vacancies in hospitals at that time.
- The patient was discharged after that and is currently doing fine.
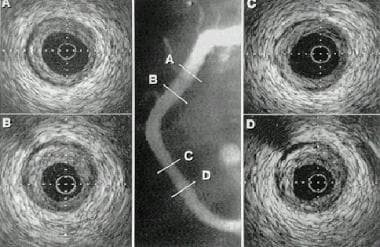
DETAILS ABOUT PCI:Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a nonsurgical technique for treating obstructive coronary artery disease, including unstable angina, acute myocardial infarction (MI), and multivessel coronary artery disease (CAD).
This is an example of PTCA.
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)Non–ST-elevation acute coronary syndrome (NSTE-ACS)Unstable angina.Stable angina.Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)High risk stress test findings. CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.Absence of cardiac surgery backup.Hypercoagulable state.High-grade chronic kidney disease.Chronic total occlusion of SVG.An artery with a diameter of <1.5 mm.In this case a PCI was not done due to non availability of vacancies in higher centres due to the ongoing pandemic. Instead she was sent home with a prescription.
QUESTION 3
Q3) (Testing peer review competency of the examinees) :
Please go through the cases in the links shared below and provide your critical appraisal of the captured data in terms of completeness, correctness and ability to provide useful leads to analyze the diagnostic and therapeutic uncertainties around the cases shared.
MULTISYSTEM:
CNS :
Renal :
Captured by one student from 2017 batch in the link below :
CVS :
Captured by one student from 2019 batch in the link below :
Abdominal :
ANSWER-
MULTISYSTEM- The case has been presented very clearly . The history taking and examination has been done precisely , providing all required information for the reader to understand the case . All the associated clinical pictures have also been provided. The data provided is correct and complete.
CNS-The case has been written precisely and in separate paragraphs , that make it easy to understand . All the required information pertaining to the case has been included. It is well organized and updated. The data provided is correct.
RENAL-The data provided is correct . But lack the discharge summary.
CVS- The case has been presented very clearly and to the point . All the data pertaining to the case has been provided . History taking and all the other investigations carried out have been done and presented meticulously .
ABDOMINAL -The data provided is correct . The discharge summary has not been provided and the case has not been updated after 23 June 2021.
QUESTION 4
Testing scholarship competency of the examinees ( ability to read comprehend, analyze, reflect upon and discuss captured patient centered data as in their 'original' answers to the assignment for May 2021):
Please analyze the above linked patient data by first preparing a problem list for each patient (based on the shared data) and then discuss the diagnostic and therapeutic uncertainty around solving those problems. Also include the review of literature around sensitivity and specificity of the diagnostic interventions mentioned and same around efficacy of the therapeutic interventions mentioned for each patient.
ANSWER-
MULTISYSTEM CASE
Problem list-
Chief complaint- Lower back pain . fever , yellowish discolouration of the eyes, 2 episodes of vomiting , three episodes of loose stool and blood in urine .
Investigations-
- Icterus present
- Creatinine in urine - 0.6mg/dl (normal -0.9-1.3mg/dl)
- Sodium in plasma - 132mEq/L (normal -136-145mEq/L)
- pCo2- 17.4 mmHg (normal-35-45mmHg)
- pO2- 119 mmHg (normal-85-95 mmHg)
- pH- 7.26 (normal - 7.35-7.45)
- Hemogram -MCV-73.2fl (normal -83-101fl)
- MCH-25.7pg(normal-27-32pg)
- MCHC-35.1%(normal - 31.5-34.5%)
- RBC count- 6.39millions/cumm (normal- 4.5-5.5 million / cumm)
- Prothrombin time - 24 seconds
- Ketone bodies present in urine
- HbA1c- 6.6%
- Urine- acidic , excess albumin content, and sugar.
- C reactive proteins- elevated
- COVID 19 antibodies - present
- Total and direct bilirubin are elevated .
- Liver enzymes are elevated .
- Total serum proteins are low.
DIAGNOSIS-Acute fulminant hepatic failure secondary to post infection with hepatic encephalopathy
CNS CASE
Chief complaint- Sudden fall followed by weakness of both the lower limbs, loss of hand grip 10 days ago, bowel and bowel incontinence.
Examination-
- Known case of tuberculosis infection
- Tone of the lower limbs -bilaterally increased
- Reflexes -reduced bilaterally in supinator muscles of the lower limb
Investigations-
- serum sodium -134 mEq/L
- serum chloride- 96 mEq/L
- Lymphocytes - 14% (normal- 20-40 percent)
- MRI of the brain with cervical spine -
- There is significant erosion of the inferior endplate of C5 and superior endplate of C6 along with intervening disc.
- An epidural abscess is seen at the level of C5-C6 that is causing the spinal cord compression and posterior displacement of the cord.
- Cord oedema is present
- Prevertebral collection extending from C2 to D3 - suggestive of anterior sub ligamentous spread.
DIAGNOSIS-Quadreparesis secondary to infectious spondylitis of C4, C5, C6, C7 and D1with epidural abscess at C5- C6.
RENAL CASE
Chief complaint- Altered sensorium, morning lethargy, fever 10 days ago, Pedal oedema with anasarca and shortness of breath even at rest.
Investigations-
- History of hypertension .
- Known case of chronic kidney disease .
- ECG - Sinus Rhythm
- Nonspecific T wave abnormality
- Borderline echo
- Hb - 12 g/dl (normal - 13- 17 g/dl)
- Lymphocytes- 11% which is much less than the normal range
- Urine examination- Albumin seen
- Ultrasound report -
- CMD partially lost in the right kidney
- Grade II fatty liver
- Simple renal cyst
- Grade II -III Renal parenchymal disorder
DIAGNOSIS-Hypertensive nephropathy with uremic encephalopathy.
CVS CASE
Chief complaint-Distension of abdomen and shortness of breath since 5days
Investigations-
- Hypothyroidism
- Bradycardia
- Hb - 10.3 gm/dl (normal-
- PCV-32.1vol% (normal- 36- 46 vol%)
- MCV-80fl (83-101fl
- MCH - 25.8 pg(27-32pg)
- HbA1c- 6.7 percent
- ECG abnormal -
- 2d- ECHO - Pleural effusion , Mild Pericardial effusion
DIAGNOSIS- HFrEF with atrial fibrillation secondary to IHD.
ABDOMINAL CASE
Chief complaint- pedal edema since 10 days, decreased urine output and burning micturition since 10 days and fever since 10 days.
Investigations-
- Known case of DM type 2, acute kidney injury secondary to urosepsis
- High Blood Pressure - 170-110 mmHg
- Pulse rate - 111 beats per minute - Tachycardia
- on complete urine examination - albumin levels were present
- Ultrasound Examination - Right kidney had grade I Renal parenchymal disease , Left kidney had Grade II Renal parenchymal Disease
- Raised serum creatinine - 3.4 mg/dl
- Raised Blood Urea- 65 mg/dl
- Serum electrolytes - Potassium level raised - 5.3 mEq /L
DIAGNOSIS-Acute kidney injury secondary to urosepsis with hyperkalemia.
QUESTION 5
Testing scholarship competency in logging reflective observations on your concrete experiences of this last month :
Reflective logging of one's own experiences is a vital tool toward competency development in medical education and research.
ANSWER-
Reflective logging enable the student to stay up to date and keep a track of their progress . They enable one to apply their theoretical knowledge into practical application.In the times of COVID when we are unable to physically attend clinical posting and acquiring practical knowledge ,elogs enable us to keeping a track of the patient assigned and practice important skills like history taking .
This helped me to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Reflective logging give us an opportunity to know the patient and study the case, inspite of us not being in the hospital.







Comments
Post a Comment